Pain from the nervous system
A success rate exceeding 70% for the treatment of certain neuropathic pain conditions can be expected when the diagnosis is clearly established based on an understanding of the mechanism
The main problem is differentiating true neuropathic pain from referred pain that usually arises from musculoskeletal structures (this pain will not respond to drugs like Lyrica).The investigation and treatment of neuropathic pain (pain with its origin in the central and peripheral nervous system) remains a major challenge. The diagnostic work-up is complex with an important proportion of pathologies involving finer nerve fibers. This makes objective documentation difficult. Many patients are treated with anti-epilectic or anti-depressant drugs for pain radiating into an arm or a leg, despite the fact that only about 20% of radiating pain is truly neuropathic (approximately 80% is referred). This explains the poor results from pharmacological treatments and the over-prescription of drugs like Lyrica.
Anti-depressants and anti-epilectic drugs such as Lyrica produce a modest (30-40%) reduction of pain in about one third of patients with proven neuropathic pain. If we estimate that only 20 out of 100 patients treated with Lyrica have true neuropathic pain, there will be only 7 responders (30-40% of 20).A one-year prescription of Lyrica at 150 mg twice daily costs 1100 CHF in Switzerland. The total cost for the 100 patients is thus 110,000 CHF/year, of which only 7700 CHF actually do any good, providing benefit for the 7 responders. This means that if 93 patients out of 100 are unlikely to respond, then 102,000 CHF are wasted, providing benefit only to the pharmaceutical company that manufactures the drug!
We therefore find it reasonable to propose to our patients that a more elaborate investigation program is justified, rather than just assuming that radiating pain is neuropathic, before introducing any therapy. The treatment should of course be decided upon after identification of the cause and clarification of the mechanism that is producing the radiating pain that has been diagnosed as possibly neuropathic from the symptoms alone.
Different pathologies producing peripheral or central neuropathic pain
Disc hernias and traumatic nerve injuries
A spinal nerve foot may be irreversibly damaged by a disc hernia, in particular when this is localized outside the spinal canal. Spinal cord stimulation (SCS) provides the most effective therapy with a success rate in the order of 70% if the patients are selected from a carefully designed pre-implantation test protocol.
A nerve root or a peripheral nerve can also be damaged by trauma, for instance a fracture or a needle. Stimulation of the damaged nerve root is often efficacious.

SCS electrode introduced into the lower thoracic epidural space for palliative treatment of nerve root pain after a lumbar disc hernia which has not improved following surgery.
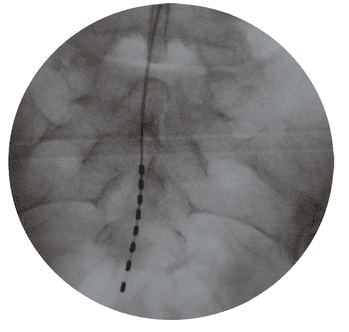
Stimulation electrode implanted in the sacral canal to treat pain from the S4 nerve root on the left side provoked by a sacral fracture after a fall.
Neuropathic pain after surgical intervention
Certain interventions in general, thoracic, gynecologic and orthopedic surgeries are associated with a high incidence of neuropathic pain conditions, usually unrecognized by the surgical community. Operations for knee prosthesis, shoulder surgery, cardiac and chest surgery, operations for inguinal hernia, cesarian section, and placement of nets to reinforce the abdominal wall are particularly common as causes for neuropathic pain starting in the postoperative period. We see about 60 new patients with such pathologies annually. They are caused either by placement of a suture around a nerve, a neuroma following a section of a nerve or by entrapment of a nerve in scar tissue. In all these conditions, we advise the patient to undergo a microsurgical revision of the operating scar, but only after we have identified the precise anatomical origin and mechanism of the neuropathic pain. A success rate of at least 80% can be expected.
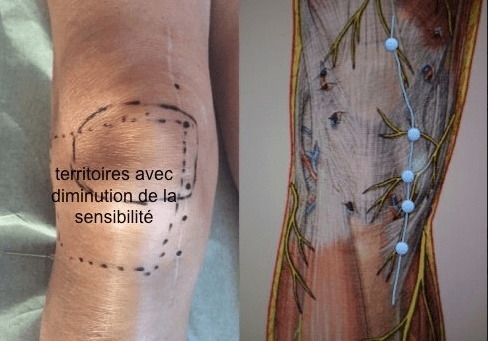
Multiple scar neuromas with start of neuropathic pain a couple of weeks after implantation of a prosthesis in the right knee.
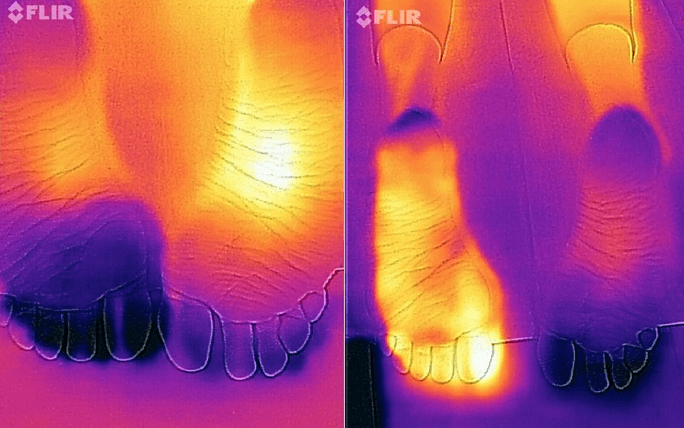
Thermography of the feet demonstrating markedly decreased skin temperature in the forefoot on the left side after reconstructive orthopedic surgery with entrapment of two interdigital nerves in deep scar tissue (left panel). After a selective sympathetic local anesthetic block, the pain disappeared along with the marked increase in temperature (right panel).
Polyneuropathies
This a degenerative disease of the peripheral nervous system, most commonly producing pain in the feet and lower legs. The type of nerve fibers causing the pain can be tested with a bedside neurological examination, for instance a thermotest. This pathology is particularly common in patients with diabetes, high alcohol intake, malnutrition, and those who have received chemotherapy. Different drugs are tested to see if the pain responds. In patients with strong pain and lack of response to medication, SCS can be tested. The success rate of SCS is 40-50%.
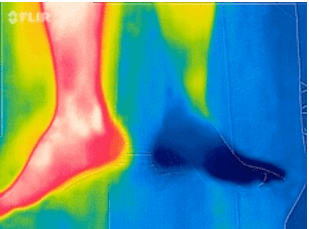
Thermography of the legs of a patient suffering severe central neuropathic pain in the left lower leg and foot along with reduced blood flow and temperature after bleeding in the deep brain (hypothalamus).
Central neuropathic pain
Pain conditions from the central nervous system are difficult to treat. They may be the consequence of cerebrovascular accidents, long-standing compression of the spinal cord in the cervical or thoracic regions, or damage to the brachial or lumbar nerve plexus caused by trauma.
Functional neurosurgical interventions such as motor cortex stimulation and cordotomies are some of the techniques used to treat central neuropathic pain. After having identified the precise mechanism of these pain conditions, we refer the patient to a university neurosurgical department competent in this area..

