Spinal pain
Different spinal pain conditions treated at the pain clinic in lausanne
If you recognise yourself among the exemples of spinal pain conditions presented below, you can contact us for an appointment with the objective of obtaining a precise diagnosis and a proposal for therapy. You can also contact us for a second opinion if you wish, even when a specific treatment has already been proposed.
Pain provoked by facet joint arthritis (joints between the vertebrae):
The success rate of radiofrequency denervation when these joints have been identifies as the sources of pain is 60-85%, depending on the region (thoracic, lumbar and cervical spine), and 75% of initially successfully treated patients will have permanent pain reduction.
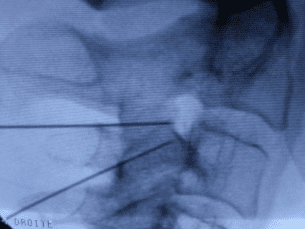
Radiofrequency denervation of the two nerves supplying the C2/C3 joint on the right side.
Neck pain after trauma (whiplash or other injury or strain):
Facet joint pathology represents 50% of neck pain following whiplash injuries and can be treated with radiofrequency denervation, resulting in around 85% success rate at one year. 20% of patients with pain after whiplash have pain from an intervertebral disc for which the only possible treatment is surgery.
Cervical headache:
Predominantly one-sided headache may have its origin in the three uppermost cervical facet joints. The most common level is C2-3 followed by C1-2.
The C1-2 joint cannot be treated with radiofrequency denervation because of the vascular anatomy at this level. This joint is commonly the origin of pain due to inflammatory disease, for instance rheumatoid arthritis, with excellent long-term response to a steroid injection into the joint. If pain is due to a mechanical problem, steroids are inefficient and surgery has to be considered.
Headache originating from the C2/C3 joint is treated with radiofrequency denervation usually with excellent results (as described above).
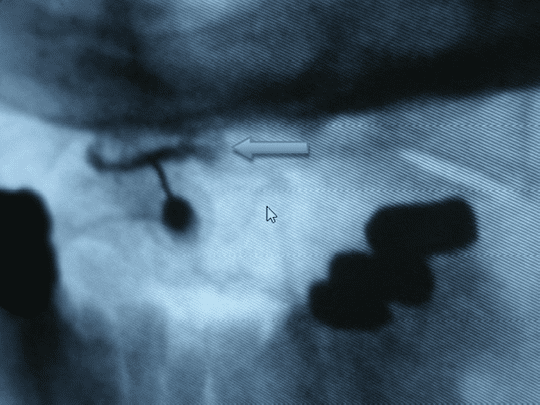
Radiological contrast injected into the left C1/C2 facet joint, severely damaged by rheumatoid arthritis.

Cervical disc hernia C5/C6
Discopathies
Cervical disc hernias:
The natural history of a cervical disc hernia is benign with over 90% spontaneous recovery within 2-3 months after onset of pain as long as there is no sign of neurological involvement (loss of power in the arm). Around 80% of patients have pain provoked by an inflammatory reaction to the disc materials expelled from the disc and are likely to respond well to oral steroids. Patients with neurological involvement should consult a neurosurgeon as soon as possible to establish if there is any indication for surgery since a delay to operate might induce irreversible nerve root damage.
Injection of steroids around the nerve root affected by the disc hernia is rarely indicated but should be considered in case of severe pain despite oral steroids. This procedure should only be performed by an experienced pain physician with skilled and diligent training in minimally invasive cervical procedures.
Thoracic disc hernias:
This is an unusual pathology for which there is a lack of information as regards success rate of any therapy. Emergency spinal surgery is indicated for a thoracic disc hernia that produces weakness in the lower extremities or urinary/fecal incontinence.
Left-sided extraforaminal disc hernia
Lumbar disc hernias:
Similar to the cervical region, most pain provoked by a lumbar disc hernia is inflammatory in origin with an incidence of around 80% and is most likely to resolve spontaneously. If leg pain is severe, it is logical to inject steroids around the affected nerve root. The success rate is around 70%, with the exception of intraforaminal or extraforaminal hernias, where pain responds poorly to steroids, since it is often mechanical rather than inflammatory in origin. These are also associated with a significant proportion of irreversible root injury.
Large disc hernia L5/S1 in the spinal canal on the left side
Internal discopathies:
IDD – Internal Disc Disruption
This pathology represents around 80% of the causes of low back pain in younger patients (20-50y), in particular among blue collar workers. lDD cannot be diagnosed by standard X-rays or MRI. A disc provocation in the form of a discography is required to establish if the origin of the low back pain is a disc. Often, these patients have several discs that are pathological, as seen on MRI. Since therapy is principally surgical, it is therefore necessary to identify which disc(s) is (are) responsible for the pain to allow the surgeon to make the right strategic decision. The use of provocation discography can improve the success rate of spinal surgery for chronic low back pain. We assist a large number of surgeons in Switzerland with data from disc provocation testing and other minimally invasive tests deemed necessary, before spinal surgery.
Degenerative disc disease
This pathology is very common in patients above the age of 50. These degenerated discs rarely cause chronic low back pain (<20%). However, disc provocation testing is used to identify the ones that are a cause of pain. In elderly patients it is much more common for low back pain to be caused by degenerative disease in the facet joints or by instability between vertebrae. When spinal surgery is considered for patients with chronic low back pain and degenerative disc disease, the same minimally invasive evaluation techniques as for IDD are recommended.
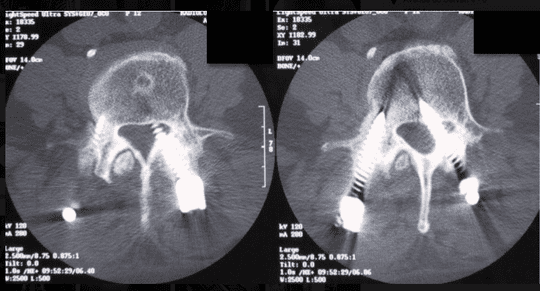
Internal rupture of the disc L4/L5 at 4 o'clock with circumferential distribution of radiological contrast (in white on the CT)
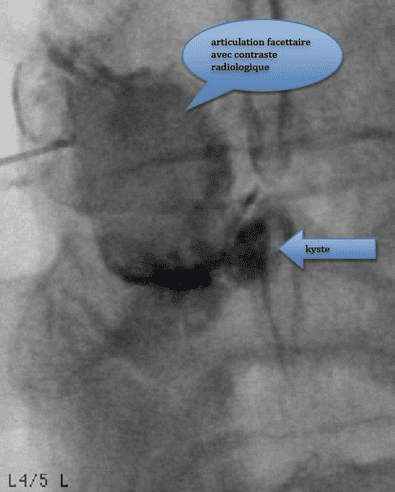
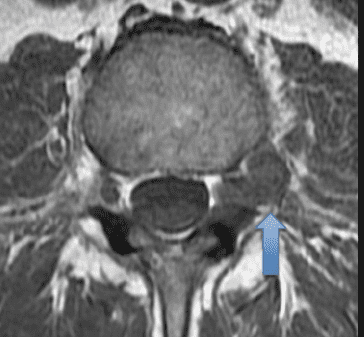
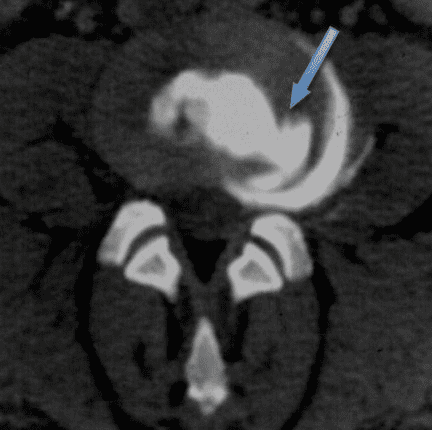
Facet joint cyst L4/L5 on the left side provoking severe L5 sciatica
Facet joint cysts:
This pathology is usually discovered on MRI following a sudden onset of severe sciatica. 75-80% of all cysts are at the level of L4/L5. The preferred treatment is by repeat cyst punctures and instillation of steroids inside the joint capsule responsible for the cyst. The cyst formation is often a consequence of inflammation due to instability in the segment, a problem to be considered if surgery is required, when the anatomical localisation of the cyst precludes access with the puncture needle (5% of patients with facet joint cysts).
Spinal stenosis:
Pain in the lower extremity (ies) on walking is the classic symtom of spinal stenosis. If the reduction of the diameter of the canal is associated with instability or a disc hernia in the same segment, pain may start within seconds of standing up from the lying or sitting positions, in areas where pain is most commonly absent. Bending over when walking with a grocery trolley often alleviates the pain, whereas bending backward may provoke severe leg pain. Injection of steroids in the stenosed segment is efficient in around 50% of patients, but only if pain is inflammatory in origin. Pain caused by purely mechanical obstruction or by irreversible injury to the nerves in the spinal canal does not respond to steroid injections. Steroids are also inefficient in spinal stenosis caused by lipid deposits in the spinal canal.Despite a good result following steroid injections into the spinal canal, a significant proportion of patients with spinal stenosis need decompressive spinal surgery, with vertebral stabilisation, often months to years after the injection therapy.

Severe dynamic spinal stenosis with forward displacement of L3 on L4

Severe obstruction of the intraspinal nerves produced by fat deposits in the canal (in grey on the MRI)
Severe pain radiating along the segment L3 on the left side provoked by a screw through the spinal canal. Spinal cord stimulation should be tested as primary treatment.
Failed back surgery syndrome - fbss:
Failure of spinal surgery is always a catastrophe for the patient and the surgeon. Understanding the precise mechanism and pathology is the only way to progress to successful therapy. This requires a profond and often time consuming analysis including diagnostic tests. Three explanations should be considered:
- Correct preoperative diagnosis - Inadequate surgical technique
- Incorrect preoperative diagnosis - Adequate surgical technique
- Incorrect preoperative diagnosis - Inadequate surgical technique
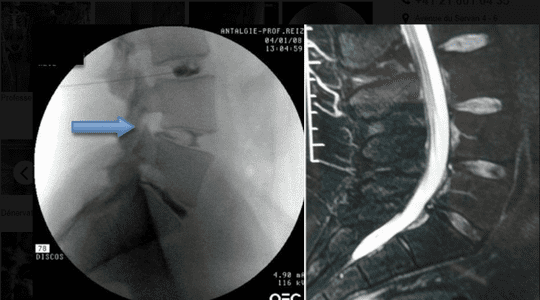
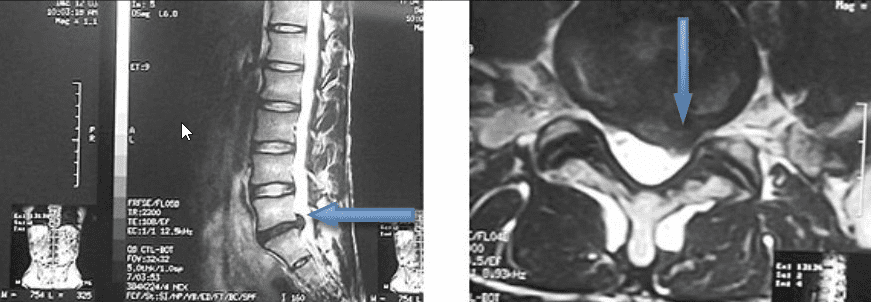
Comparison between disc provocation test (left) and MRI (right). Without the result of the preoperative disc provocation, the surgeon would not have known which disc was responsible for the back pain (L4/L5).
Prevention of FBSS:
The decision to operate for chronic low back pain is mainly made from a combination of the patient's medical history, the medical examination and a lumbar MRI. At best, this combination has a diagnostic precision of 50%, which is why, on average, the success rate is no more than 40% (according to the medical literature). The only possible way to improve the results of spinal surgery is to better identify the anatomical structures in the spine that are the cause of the pain for which surgery is intended. This can only be achieved by 'Precision Diagnostics', using the minimally invasive methods that are used routinely in our Pain Centre.

SCS electrode introduced into the lower thoracic epidural space for palliative treatment of nerve root pain after a lumbar disc hernia which has not improved following surgery.
How to understand what happened?
There are four possibilities:
- The preoperative pain has disappeared completely but a new pain started immediately or some time after surgery – it is probable that the cause of pain was correctly identified and treated, but that a complication occurred.
- The preoperative pain has completely disappeared to return exactly like before, weeks to months later – this could be a lack of consolidation of a fusion (material failure, infection, smoking) or a psychological ("placebo") benefit of the surgery.
- The preoperative pain has not changed with the intervention – preoperative diagnosis was probably incorrect.
- The preoperative pain has not decreased and in addition, there is a new pain that appeared after the intervention - incorrect preoperative diagnosis associated with a complication is the likely explanation.
How do we deal with patients with FBSS?
An in-depth consultation followed by a discussion with the responsible surgeon is necessary. Often, new radiological examinations and a bone scintigraphy are needed. Suspicions of neurological damage need to be confirmed and documented by a neurologist. Pharmacological testing methods are often used to distinguish back pain associated with radiation into a leg that is neuropathic in origin as opposed to musculoskeletal referred pain. Once we have a clear understanding of the origin(s) of the pain we can choose between the possible therapeutic options.
A new surgical intervention, for instance in the case of a non-fusion of a spondylodesis causing the pain.
Palliative pain therapy by spinal cord stimulation (SCS) in the case of predominantly neuropathic pain, or by implantation of a pump system for administering a potent analgesic when the pain is of predominantly musculoskeletal origin.

